Snakebite treatment has come a long way, but not every venom has a reliable antidote. In rare cases, a snake’s toxins are too complex, too fast-acting, or too poorly studied for antivenom to work. Some species were identified long before modern venom research even began, while others became medically significant only after repeated incidents revealed how unpredictable their poisons could be. These snakes remind us that nature still holds dangers that science hasn’t fully solved, and encountering them requires fast medical care, supportive treatment, and a respect for the limits of antivenom.
1. Boomslang (Dispholidus typus)

First described in 1850, the boomslang gained medical attention only after a 1957 fatality revealed how devastating its slow-acting hemotoxins can be. Antivenom exists but is extremely rare and often unavailable in regions where the snake lives. Its venom causes internal bleeding that may not respond to treatment unless administered immediately, making many bites effectively untreatable. Because the species’ venom varies widely across populations, producing a consistently effective antivenom has proven difficult, leaving supportive care as the primary approach.
2. Twig Snake (Thelotornis capensis)

Documented scientifically in 1874, the twig snake was long overlooked because human encounters were infrequent. Its venom causes severe hemorrhaging similar to the boomslang, yet no widely produced antivenom has ever been developed. Early attempts in the mid-1900s failed due to difficulties in safely milking the species and the limited demand for a commercial antidote. Once symptoms begin, they progress rapidly, and treatment focuses on blood transfusions and stabilizing vital signs. Because antivenom is unavailable, most cases rely solely on supportive care rather than a targeted cure.
3. Blue Coral Snake (Calliophis bivirgata)

First described in 1837, the blue coral snake gained notoriety only recently when researchers discovered its “lightning-strike” venom, which forces nerves to fire uncontrollably. Unlike traditional neurotoxins, this mechanism overwhelms the nervous system too quickly for existing antivenoms to counteract. Attempts to create a specific antidote have stalled because the venom contains unusual compounds difficult to replicate for production. Bites are rare but highly dangerous, and treatment focuses on respiratory support and managing seizures rather than neutralizing the toxins directly.
4. Spitting Cobra Variants (Certain Naja species)

Some spitting cobras were identified as far back as the early 1800s, but their evolving venom profiles have complicated antivenom development. While antivenom exists for many cobra species, several spitting populations produce cytotoxins so aggressive that tissue destruction continues even after treatment. Researchers found in the 1990s that these venoms contain fast-acting compounds that antivenom molecules struggle to bind in time. As a result, bites often lead to permanent damage despite therapy, making them essentially untreatable from a toxin-neutralization standpoint.
5. Small-Scaled Burrowing Asp (Atractaspis microlepidota)

First described in 1888, this elusive snake quickly puzzled scientists with its sideways-striking fangs and extremely potent venom. Attempts to create antivenom in the mid-20th century repeatedly failed because the toxins vary so drastically between populations that no single formula worked universally. The venom’s cardiovascular effects are rapid and unpredictable, leaving doctors to rely on stabilizing blood pressure and heart rhythm rather than neutralizing the toxins. With no commercial antivenom available, treatment remains supportive and often challenging.
6. Rough-Scaled Bush Viper (Atheris hispida)

Discovered in 1955, this striking viper lives in isolated, mountainous regions where medical research has been historically limited. Its venom composition remains poorly studied, and no dedicated antivenom has been produced. Efforts in the 1990s to test cross-reactivity with existing viper antivenoms showed inconsistent and largely ineffective results. Because the toxins can cause rapid organ stress and severe clotting issues, care focuses on symptom management rather than neutralization. The lack of reliable antivenom makes each bite medically unpredictable.
7. Malayan Blue Krait (Bungarus candidus)

Formally described in 1936, the Malayan blue krait carries neurotoxins far more potent than many related species. Although some general krait antivenoms exist, they often fail to bind effectively to this snake’s unique toxins. The venom shuts down the nervous system quietly and quickly, sometimes before treatment is even considered. Field reports from the late 20th century revealed frequent antivenom failures, prompting doctors to focus instead on ventilatory support until the toxins wear off. Survival depends heavily on rapid hospitalization rather than antivenom success.
8. Many-Horned Adder (Bitis cornuta)
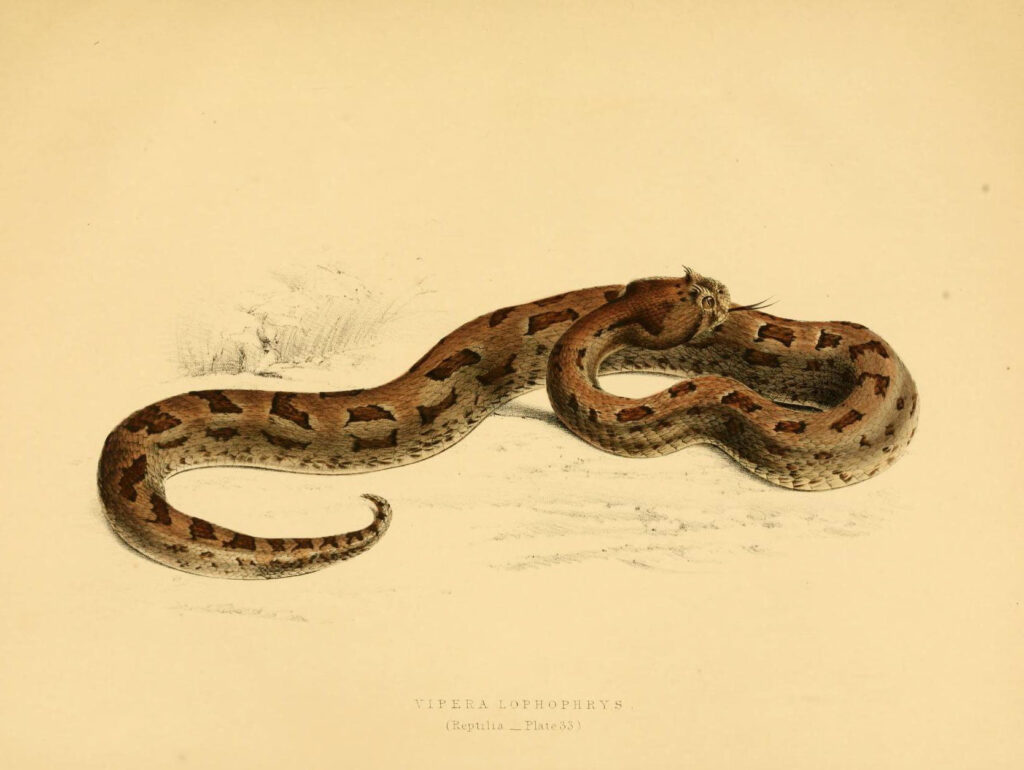
Identified in 1826, the many-horned adder has long been recognized for its unpredictable venom, which varies significantly across its range. No specific antivenom has been developed, and trials using related viper antivenoms have shown limited effectiveness. The snake’s toxins can cause intense swelling, clotting issues, and tissue damage that progress even with aggressive medical care. Because creating a dedicated antivenom has never been commercially viable, treatment relies on wound care, hydration, and careful monitoring, making its bites effectively untreatable from an antivenom standpoint.
Comments